Introduction to Rhinoplasty
The roots of rhinoplasty date back to ancient times, with initial procedures being more about restoration rather than cosmetic alteration. Over the years, the development of new techniques and a better understanding of nasal anatomy have allowed for more sophisticated and predictable results.
Typically, the procedure can address a range of concerns, including but not limited to, the overall size of the nose in relation to facial balance, the width of the nose at the bridge, the appearance of humps or depressions on the bridge, nasal tip shape and size, nostril size and position, and asymmetry or deviation.

The roots of rhinoplasty date back to ancient times, with initial procedures being more about restoration rather than cosmetic alteration. Over the years, the development of new techniques and a better understanding of nasal anatomy have allowed for more sophisticated and predictable results.
Typically, the procedure can address a range of concerns, including but not limited to, the overall size of the nose in relation to facial balance, the width of the nose at the bridge, the appearance of humps or depressions on the bridge, nasal tip shape and size, nostril size and position, and asymmetry or deviation.

Rhinoplasty can be performed for aesthetic reasons, functional reasons, or a combination of both. Aesthetic rhinoplasty focuses on the appearance and seeks to create balance and symmetry. Functional rhinoplasty is performed to repair the nose’s structure to improve breathing. treatment.
Whether it’s to reshape what nature has provided, repair damage from an accident or injury, or alleviate structural issues that impede breathing, rhinoplasty offers a solution tailored to each individual’s goals and needs. It’s important for anyone considering this procedure to have a clear understanding of the potential outcomes, to hold realistic expectations, and to choose a surgeon who is board-certified and specializes in this type of surgery.
The Science Behind Rhinoplasty
Rhinoplasty isn’t just a cosmetic procedure but also a complex surgical practice that involves a deep understanding of facial anatomy, particularly the nasal structure. The nose’s intricate anatomy comprises bone, cartilage, and soft tissues, which together define its size, shape, and function. Surgeons must consider not only the external aesthetic but also the internal mechanics that contribute to airflow and breathing.
The procedure begins with a thorough examination of the internal nasal structures, including the septum, turbinates, and nasal valves, to ensure that any functional issues are identified and addressed. The septum, the wall dividing the nasal passages, can often be deviated, leading to obstruction and impaired breathing. Turbinates, the structures inside the nose that humidify and filter the air we breathe, can sometimes be enlarged, contributing to airflow restriction. Addressing these issues is a crucial part of functional rhinoplasty.
In terms of the external structure, the upper portion of the nose is bone, while the lower portion is primarily cartilage. Rhinoplasty can involve reshaping or altering these structures to achieve the desired outcome. This may include breaking and repositioning the bone (osteotomy), reshaping the cartilage, or adding grafts to provide additional support and shape.
The skin covering the nose is also a critical factor; its thickness and elasticity can influence the surgery’s results. Thicker skin may conceal subtle changes and can be more prone to swelling, while thinner skin may show imperfections more readily.
Surgeons also employ advanced computer imaging technology to help patients visualize potential results before surgery, although it’s important to note that these images serve as a guide rather than a guarantee of the outcome.
Advancements in the field of rhinoplasty continue to evolve, with a trend towards more conservative and individualized approaches that prioritize natural results and maintain, or enhance, the nose’s functional capacity. Surgeons now emphasize preserving as much of the original structure as possible, reinforcing the existing framework rather than reducing it, and ensuring that changes made are in harmony with the patient’s other facial features.
Understanding Nasal Anatomy
-
External Anatomy
Nasal Bridge : The bony top part of the nose that connects to the forehead.
Nasal Tip : The protruding end of the nose formed by the nasal tip cartilages.
Nostrils : The openings for air passage, which are divided by the columella. -
Internal Anatomy
Septum :A partition made of cartilage and bone that separates the two nasal cavities.
Turbinates : Curved bone structures covered with tissue that warm and humidify the air.
Nasal Cavities: The space within the nose lined with mucous membranes and cilia (tiny hairs) to filter dust and pathogens.
Sinuses: Air-filled spaces in the bones of the face that are connected to the nasal cavity. -
Functionality
The nose serves multiple functions, including:
Breathing : The primary pathway for inhaling and exhaling air.
Filtering : The nasal hair and mucous membranes trap particles and pathogens.
Humidifying : The turbinates add moisture to the air to prevent dryness in the respiratory system.
Temperature Control: The air is warmed or cooled to body temperature before reaching the lungs.
Olfaction: The sense of smell occurs as air passes over the olfactory receptors in the upper nasal cavity.
Surgeons must evaluate the patient’s unique nasal anatomy in detail before the procedure, considering factors like skin thickness, the strength of cartilage, and the relationship of the nasal structures to the rest of the face. This thorough understanding of nasal anatomy helps ensure that results are not only aesthetically pleasing but also maintain or improve nasal functionality.
Reasons for Rhinoplasty
-
Cosmetic Reasons
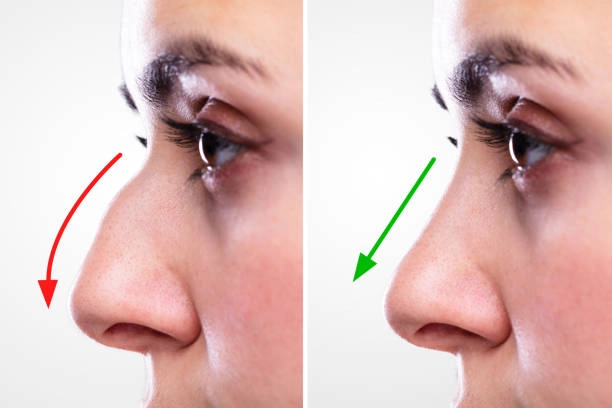
Reshaping the Nose : Individuals may desire a change in the size, shape, or angles of their nose to enhance facial harmony.
Nasal Tip Refinement : Altering the tip of the nose to be less bulbous, more refined, or better aligned with the rest of the facial features.
Correcting Asymmetry: Addressing any natural or injury-induced asymmetries for a more balanced appearance.
Profile Alterations: Smoothing out bumps on the nasal bridge or adjusting the slope of the nose.
Proportion Adjustments: Ensuring the nose is in proportion to other facial features, taking into account factors like facial width and height. -
Functional Reasons
Improving Breathing:Correcting structural issues such as a deviated septum that can cause breathing difficulties.
Repairing Damage: Restoring the nose's structure and function following an injury or trauma.
Congenital Defects: Addressing birth defects that affect both the appearance and function of the nose. -
Reconstructive Reasons
Post-Cancer Surgery:Rebuilding the nose after surgical removal of skin cancers or other diseases.
Secondary Rhinoplasty: Correcting or improving the results of a previous rhinoplasty procedure. -
Psychological and Emotional Reasons
Self-Esteem:Enhancing one’s self-image and confidence if they are self-conscious about their nose.
Social Concerns: Addressing bullying or teasing due to the nose's shape or size.
Types of Rhinoplasty Procedures


1. Open Rhinoplasty
- Involves an incision across the columella (the small strip of skin between the nostrils).
- Provides the surgeon with a direct view of and access to the underlying structures.
- Typically used for more complex cases where extensive reshaping is needed.
2. Closed Rhinoplasty
- All incisions are made within the nostrils, resulting in no visible scarring.
- Offers limited access compared to open rhinoplasty, but with less post-operative swelling and a quicker recovery time.
- Suitable for patients requiring minor adjustments.
3. Revision Rhinoplasty
- Also known as secondary rhinoplasty, performed to correct or improve the results of a previous nose surgery.
- Can be more complex due to the changes in the nasal structure from the initial surgery.
4. Filler Rhinoplasty
- A non-surgical option that involves the use of injectable fillers to make minor corrections or enhancements to the nose.
- Temporary and less invasive but offers limited changes compared to surgical rhinoplasty
5. Functional Rhinoplasty
- Aimed at correcting structural issues that affect breathing, such as a deviated septum.
- While it can also improve the nose's appearance, the primary goal is to improve nasal function.
6. Ethnic Rhinoplasty
- Tailored to individuals of various ethnic backgrounds, respecting the unique characteristics and preserving the ethnic identity while making desired changes.
- Focuses on aesthetic balance and proportion without westernizing the nose.
7. Reduction Rhinoplasty
- Designed to reduce the size of the nose by removing bone or cartilage
- Often sought by individuals with a prominent nasal bridge bump or large nasal tip.
8. Augmentation Rhinoplasty
- Involves adding to the nasal structure, often using grafts taken from other parts of the body, to enhance or build up the nasal bridge or tip.
9. Tip Plasty
- Focuses specifically on reshaping the nasal tip without altering the rest of the nose's structure.
- Can involve either adding structure to the tip or reducing the cartilage for refinement.
The Consultation Process for Rhinoplasty

-
Initial Contact
Patients typically begin by scheduling a consultation appointment with a plastic surgeon specializing in rhinoplasty.
-
Patient's Medical History
A thorough review of the patient's medical history, including any previous nasal surgeries, allergies, and medications, to ensure safety and suitability for the surgery.
-
Discussion of Goals and Expectations
The surgeon will discuss with the patient their aesthetic goals, what changes they would like to see, and what can realistically be achieved through surgery. - It's often helpful for patients to bring photos of noses they admire or wish to emulate.
-
Physical Examination
A detailed examination of the nose's external and internal structures, including skin quality and nasal anatomy. - This helps the surgeon assess the technical aspects that need to be addressed during surgery
-
Imaging and Morphing Tools
Many surgeons use digital imaging technology to give patients a preview of potential postoperative results. - This can aid in setting realistic expectations and refining goals.
-
Explanation of the Procedure
The surgeon explains the recommended type of rhinoplasty, the techniques involved, the scope of surgery, and what to expect during recovery.
-
Risks and Complications
A discussion about the potential risks and complications associated with rhinoplasty to ensure informed consent.
-
Pre- and Post-Operative Instructions
Patients receive detailed instructions to prepare for surgery, such as stopping certain medications or smoking cessation, as well as what to expect and how to care for themselves post-surgery.
-
Cost and Financial Considerations
The cost of the procedure, including surgeon's fees, anesthesia, facility costs, and post-operative care, are outlined. Payment plans or financing options may also be discussed.
-
Question and Answer Session
Patients are encouraged to ask questions to clarify any doubts and to ensure a clear understanding of the procedure, recovery, and expected outcomes.
-
Scheduling
If the patient decides to proceed with rhinoplasty, they can schedule the surgery date. Some patients may need time to consider the information before making a decision.
-
Preoperative Clearance
Depending on the patient's age and health status, preoperative medical clearance from their general practitioner or a specialist may be required.
Preparing for Your Rhinoplasty Procedure
-
Medical Evaluation
Undergo a pre-operative medical examination to ensure you are healthy enough for surgery. Discuss with your surgeon about any routine medications and supplements you are taking.
-
Lifestyle Adjustments
If you smoke, you will need to stop at least a few weeks before the surgery, as smoking can significantly impair healing. Avoid alcohol and any anti-inflammatory drugs or herbal supplements that can increase bleeding.
-
Nutritional Preparation
Focus on a well-balanced diet to support healing; consider increasing intake of foods rich in vitamins A and C.
-
Pre-Surgery Planning
Arrange for someone to drive you to and from surgery, and for someone to stay with you for at least the first night after the procedure.
-
Home Preparation
Stock up on groceries and easy-to-prepare meals, as well as any prescriptions you may need post-operatively. Set up a comfortable recovery area where you can rest with your head elevated.
-
Follow Pre-Operative Instructions
Your surgeon may provide specific instructions regarding eating, drinking, and taking certain medications on the day before and the day of surgery.
-
Mental Preparation
It’s normal to feel a bit anxious before your procedure. Consider relaxation techniques such as deep breathing, meditation, or talking to a friend or counselor to ease any pre-surgery nerves.
-
Necessary Items
Have cold compresses ready for use after surgery to help reduce swelling. Purchase any recommended aftercare supplies, like saline nasal spray and lip balm.
-
Clothing
Prepare loose-fitting, comfortable clothes that do not need to be pulled over your head.
-
Fasting
Typically, you will be instructed to not eat or drink after midnight on the night before your surgery.
-
Contact Numbers
Ensure you have all necessary contact numbers for your surgeon or the surgical facility in case of any last-minute questions or concerns.
-
Post-Surgery Appointments
Schedule your follow-up appointments beforehand so that you can focus on recovery after the procedure.
The Rhinoplasty Procedure
-
Anesthesia
The procedure typically begins with the administration of anesthesia, which can be local with sedation or general, depending on the complexity of the surgery and your surgeon's recommendation.
-
Incision
Open Rhinoplasty : An incision is made across the columella, the narrow strip of tissue that separates the nostrils, providing the surgeon with a direct view of the nasal structures. Closed Rhinoplasty : Incisions are hidden inside the nose, resulting in no visible scarring.
-
Reshaping the Nose Structure
For a nose that's too large, the surgeon may remove bone or cartilage to achieve the desired size. In cases where the nose needs to be augmented, cartilage grafts, often taken from the septum, ear, or ribs, are used.
-
Correcting a Deviated Septum
If the septum is deviated, it can be straightened, and the projections inside the nose reduced to improve breathing.
-
Closing the Incision
Once the nose is sculpted to the desired shape, the skin and tissue are redraped, and the incisions are closed with sutures. Additional stitches may be placed in the natural creases of the nostrils to refine the new shape.
-
Observing the Results
The surgeon may place a splint on the nose to support and protect the new structures during the initial healing phase. In some cases, nasal packs or soft splints might be placed inside the nostrils to stabilize the septum.
-
Immediate Post-Operative Phase
After the surgery, you'll be monitored in a recovery room where your immediate post-operative condition will be closely observed. Once your condition is stable, you may be allowed to go home the same day, which is common in outpatient procedures.
-
Recovery Time
Initial swelling and bruising around the eyes and nose will generally improve after the first week. It may take several weeks for most of the swelling to subside and up to a year for the new nasal contour to fully refine.
-
Follow-Up Visits
Regular follow-up visits will be scheduled to monitor your healing progress and address any concerns.
Recovery and Healing after Rhinoplasty
-
Post-Surgery Care
Immediately following surgery, patients may experience swelling, bruising, and some discomfort. Pain is typically manageable with prescribed medications. A nasal splint is usually required for the first week after surgery to protect the nasal structures.
-
Managing Swelling and Bruising
Applying cold compresses around, but not directly on, the nose can help reduce swelling. Keeping the head elevated, even when sleeping, is recommended for the first few days to minimize swelling.
-
Activity Restrictions
Strenuous activities and exercises should be avoided for at least 3 to 6 weeks. It’s important to avoid any blows to the nose during the recovery period.
-
Follow-Up Visits
Surgeons typically schedule postoperative visits to remove sutures, check on the healing process, and address any concerns.
-
Visible Changes and Healing Time
While initial changes are noticeable almost immediately, the final shape of the nose may take up to a year to fully develop. Internal healing also continues for several months after the procedure.
-
Sensations During Healing
Patients may experience numbness or changes in skin sensation; these usually improve within the first few months.
-
Scar Care
If an open rhinoplasty was performed, care instructions for the small scar at the base of the nose will be provided. Scars typically fade significantly with time and proper care.
-
Long-term Care
Protection from the sun is advised to prevent skin discoloration, especially in the first year following surgery. It’s important to follow a healthy lifestyle to support the healing process and maintain results.
-
Emotional Healing
Emotional fluctuations are common post-surgery, and it’s important to have a support system in place. Communicating with your surgeon about any concerns is crucial for emotional and physical recovery.
-
Understanding Results
Patience is key, as the final result is not immediately apparent due to gradual subsiding of swelling. Adjustments to the new appearance can take time, and psychological readiness for change is an important aspect of recovery
Risks and Possible Complications of Rhinoplasty

-
Anesthetic Complications
Reactions to anesthesia can occur, ranging from mild nausea to more serious allergic reactions.
-
Bleeding
Some bleeding is normal after surgery, but excessive bleeding may occur and could require additional treatment.
-
Infection
While uncommon due to stringent sterilization practices, infections can happen and may necessitate antibiotics or further surgery.
-
Scarring
Any surgery leaves scars, but in rhinoplasty, they are usually inside the nose. In the case of an open rhinoplasty, scars at the base of the nose may be visible but typically fade over time.
-
Breathing Difficulties
Changes made during surgery can affect nasal airflow, potentially resulting in breathing difficulty which may require additional surgery to correct.
-
Dissatisfaction with Aesthetic Outcome
Some patients may not be satisfied with the results. Revision surgery may be an option in some cases.
-
Numbness or Altered Sensation
Numbness around the nose or altered sensation may occur, which usually improves over time but can be permanent in rare cases.
-
Prolonged Swelling
Some patients may experience prolonged swelling, taking up to a year to fully subside.
-
Septal Perforation
A hole in the nasal septum can develop, potentially causing chronic nosebleeds, whistling when breathing, and breathing difficulty.
-
Need for Revision Surgery
Additional surgery may be necessary if the initial outcome is not as expected or if complications arise.
-
Psychological Impact
The emotional impact of a changed appearance can be significant, and some patients may experience psychological distress.
Post-Surgery Considerations for Rhinoplasty
-
Immediate Aftercare
Post-operative instructions must be followed closely, such as how to care for the nasal area and sutures, medications to take to aid healing and reduce the risk of infection, and when to return for a follow-up appointment.
-
Rest and Recovery Time
Adequate rest is essential. The first few days after surgery should involve minimal activity. Patients typically need to take one to two weeks off work and avoid strenuous activities for up to six weeks.
-
Swelling and Bruising
Swelling and bruising are common and can last several weeks. Applying cold compresses and keeping the head elevated can help reduce swelling.
-
Nasal Packing and Splints
Nasal packing is often used to control bleeding, and splints may be placed to stabilize the nose. These are usually removed within a week after surgery.
-
Managing Pain and Discomfort
Pain, which can vary in intensity, is typically managed with prescribed or over-the-counter pain relievers.
-
Avoiding Certain Facial Expressions
Patients are advised to limit facial expressions and movements that put pressure on the nose.
-
Protecting the Nose
The nose will be more susceptible to injury after surgery, so protecting it from accidental bumps is crucial. Wearing glasses may also need to be limited or adjusted.
-
Long-term Care
Long-term follow-up care may involve occasional visits to the surgeon to monitor the progress of healing.
-
Sun Protection
Protecting the nose from the sun to prevent skin discoloration and to aid in the healing process is important. Use high-SPF sunscreen and wear hats when outdoors.
-
Patience with Final Results
It may take up to a year for the final results of the surgery to be fully apparent due to residual swelling.
-
Psychological Adjustment
Adjusting to the new appearance can take time, and patients may benefit from support from friends, family, or professional counselors.
-
Revision Surgery
If the outcome does not meet the expectations or if complications arise, revision surgery might be considered, typically after waiting for the full healing process to conclude.
Costs and Financing Options for Rhinoplasty in India
Procedure Costs
- Rhinoplasty costs can range from a more affordable end for basic procedures to a premium for more complex work or revision surgeries
- The average cost of rhinoplasty in India can be anywhere from INR 50,000 to INR 2,00,000, with variations based on individual cases.
Inclusions and Exclusions
- Understanding what is included in the quoted price is vital. Some clinics may provide an all-inclusive package that covers pre-operative tests, the surgery itself, post-operative care, and follow-up visits, while others may charge for each separately.
Additional Costs
-
Additional costs may include medications, post-surgery garments, or any unforeseen complications that require further medical intervention.
Payment Plans
-
Some clinics offer payment plans that allow patients to pay for the procedure in installments, making the surgery more accessible to a broader range of patients.
Medical Loans
-
Medical loans are available through various financial institutions in India, and they can provide patients with the necessary funds while allowing them to repay over time.
Health Insurance
-
Health insurance in India typically does not cover cosmetic procedures like rhinoplasty unless it's necessitated by a medical condition such as a deviated septum or as part of reconstructive surgery after an accident. Patients must check with their insurance providers for coverage details.
Medical Tourism Packages
-
Some healthcare providers offer comprehensive medical tourism packages that include the cost of the surgery, travel, accommodation, and sometimes even post-operative vacation options. These packages can offer savings over arranging each aspect separately.
Consultation with Multiple Clinics
-
It is advised to consult with multiple clinics to compare prices and services offered. Some clinics might provide free initial consultations, which can be beneficial for budget planning.
Quality versus Cost
-
While cost is a significant factor, it is equally important to consider the quality of care, the surgeon's expertise, and the facility's standards. Opting for the cheapest option isn’t always the best choice for surgical procedures.
Hidden Costs
-
Patients should inquire about any potential hidden costs or additional fees that could arise after the surgery to ensure they are financially prepared for the total expense.
Choosing the Right Surgeon for Rhinoplasty
-
Board Certification and Credentials
Ensure the surgeon is certified by a recognized board, such as the Board of Plastic Surgery or Otolaryngology in India. These certifications indicate that the surgeon has undergone extensive training and adheres to rigorous standards.
-
Experience and Specialization
Look for a surgeon who specializes in rhinoplasty and performs the procedure regularly. Inquire about the number of rhinoplasty surgeries they conduct each year and their experience with cases similar to yours.
-
Before and After Gallery
A reputable surgeon should have a portfolio of before and after pictures of their previous patients. This gallery can provide insight into the surgeon’s aesthetic style and the outcomes you might expect.
-
Patient Testimonials
Reading testimonials and reviews from former patients can give you a sense of the surgeon’s reputation and the satisfaction level of their clients.
-
Personal Rapport
The surgeon-patient relationship is crucial. During consultations, assess whether you feel comfortable with the surgeon. Do they listen to your concerns, explain things clearly, and make you feel at ease?
-
Hospital Affiliations
A surgeon’s affiliation with reputable hospitals can be a positive indicator of their standing in the medical community.
-
Safety and Surgical Facility
Ensure that the surgery will be performed in an accredited facility equipped to handle emergencies. The quality of the surgical facility is as crucial as the quality of the surgeon.
-
Postoperative Care
Good aftercare is essential for recovery. Find out about the follow-up care you will receive and the surgeon’s policies regarding revision surgeries, should they be necessary.
-
Professional Memberships
Memberships in professional organizations, such as the Indian Association of Aesthetic Plastic Surgeons, can indicate that a surgeon is keeping current with the latest advancements and ethical standards in their field.
-
Communication
The best surgeon is one who communicates openly, offers realistic expectations, and explains the risks and potential outcomes clearly.
-
Second Opinions
Don’t hesitate to get a second or even third opinion. It can provide different perspectives and help you feel more confident in your final decision.
-
Cost Considerations
While cost shouldn't be the sole factor in choosing a surgeon, it's essential to discuss fees upfront to avoid any hidden charges.
-
Location
Consider the location of the surgeon’s practice. While you may be willing to travel for a highly recommended surgeon, remember to consider the practicality of follow-up visits.
-
Anesthesia Team
The qualifications of the anesthetist are as important as those of the surgeon. Ensure that a certified anesthesiologist will be present during your surgery.

