Overview of Weight Loss or Bariatric Surgery
The principle behind bariatric surgery is to restrict food intake and decrease the absorption of food in the stomach and intestines. This surgical intervention is a significant consideration that requires a commitment to a new lifestyle, including a healthy diet and regular exercise, which are essential to achieve and maintain the benefits of the surgery.

While bariatric surgery can offer a fresh start for patients on their weight loss journey, it’s crucial to understand that it’s not a miracle cure. The success of the surgery is closely linked to a patient’s willingness to adopt a healthier lifestyle and follow the medical advice provided by their healthcare team.
By choosing bariatric surgery, patients are taking a proactive step towards a longer and healthier life. With the support of experienced surgeons and medical professionals, individuals can look forward to significant weight loss and the resolution or improvement of comorbid conditions, paving the way for a renewed sense of self and well-being.
Types of Bariatric Surgery
Bariatric surgery is not a one-size-fits-all procedure. There are several types of surgeries available, each with its own advantages and mechanisms of action. The following are a brief overview of the most commonly performed bariatric surgeries:
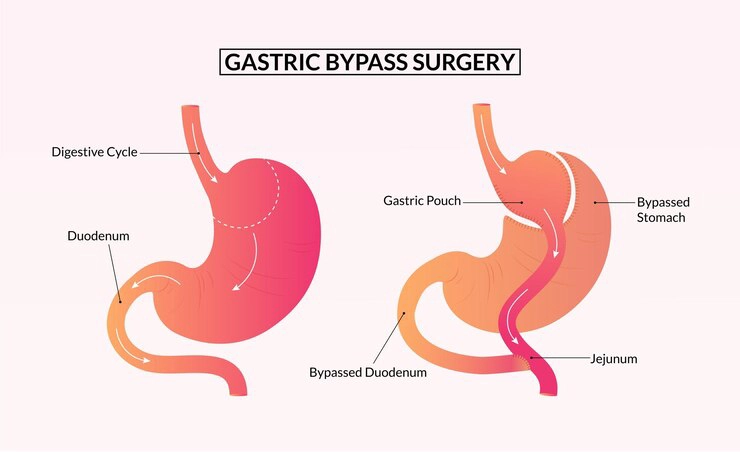
Gastric Bypass (Roux-en-Y Gastric Bypass)
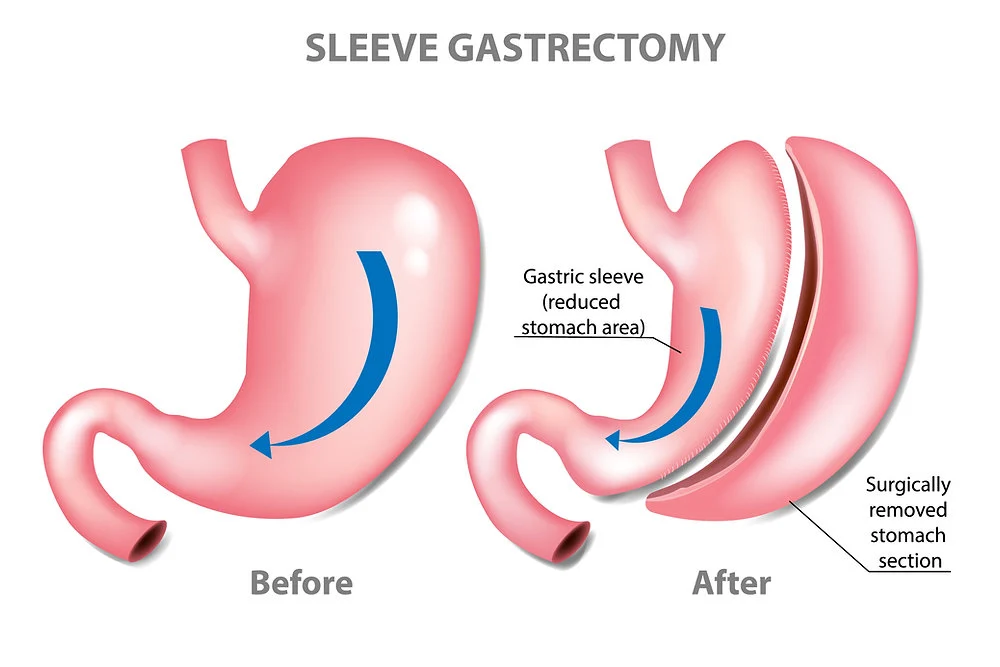
Sleeve Gastrectomy
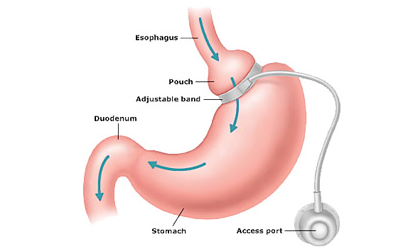
Adjustable Gastric Band
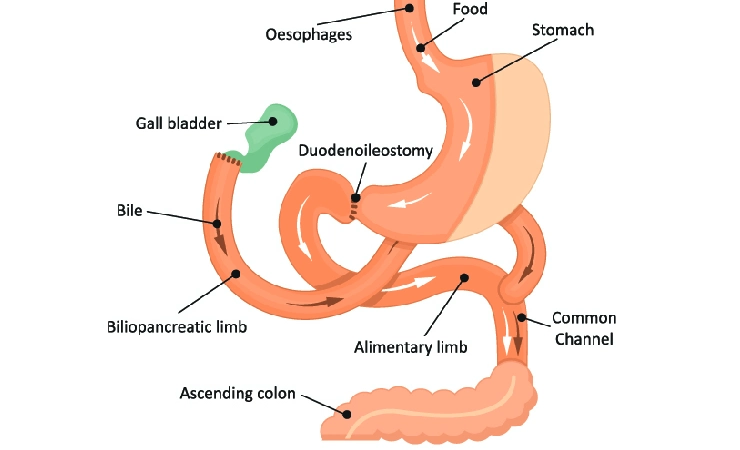
Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
Patients are encouraged to discuss these options in detail with their surgeon to understand the full scope of potential risks and outcomes. Making an informed decision is key to the success of your weight loss journey.
Who is a Candidate for Bariatric Surgery?

-
Body Mass Index (BMI):
The primary criteria for bariatric surgery is a BMI that is indicative of severe obesity. Typically, individuals with a BMI of 40 or higher are considered eligible. Those with a BMI of 35-39.9 with obesity-related health conditions may also qualify.
-
Obesity-Related Health Conditions
People with a lower BMI but who suffer from serious health problems related to obesity, such as type 2 diabetes, high blood pressure, severe sleep apnea, or other life-threatening cardiac and respiratory conditions, may also be candidates.
-
Previous Weight Loss Efforts
Candidates should have a history of failed attempts at weight loss through traditional methods like diet, exercise, and behavioral changes. Bariatric surgery is considered when these methods do not result in significant or sustainable weight loss.
-
Psychological Evaluation
Mental health stability is crucial for a successful outcome. Candidates must undergo a psychological evaluation to ensure they understand the surgery’s impact and are prepared to make lifelong lifestyle changes.
-
Commitment to Follow-Up
Long-term follow-up care is essential for monitoring health, nutritional status, and mental well-being. Candidates must be willing and able to commit to regular check-ups and possibly lifelong supplementation.
-
Understanding the Risks
A clear understanding of the potential risks and complications associated with bariatric surgery is necessary. Patients must be informed about the possible challenges and lifestyle changes required post-surgery.
-
Age Considerations
While there’s no specific age limit, candidates are generally between 18 and 65 years old. Exceptions may be made based on the individual’s specific health conditions and potential benefits from the surgery.

If you’re considering bariatric surgery, a consultation with a qualified bariatric surgeon is the first step. They will review your medical history, conduct a thorough physical exam, and discuss the best options for your unique situation.
Preparing for Bariatric Surgery
-
Medical Evaluation
A comprehensive medical exam will assess your health and identify any conditions that could affect the surgery's safety or outcome. You'll undergo tests like blood work, cardiovascular evaluation, and others based on your health needs.
-
Nutritional Counseling
Understanding the dietary changes you'll need to make before and after surgery is crucial. A registered dietitian can help you start with a pre-surgery diet to reduce fat around the liver and spleen.
-
Psychological Assessment
Mental readiness is key to adapting to the lifestyle changes post-surgery. You may need to meet with a psychologist to discuss your relationship with food and any emotional adjustments needed.
-
Education
You'll receive detailed information about the surgery, including what to expect during the procedure, the risks involved, and the recovery process. You'll learn about the lifestyle changes necessary for a successful outcome.
-
Lifestyle Changes
It's essential to quit smoking, limit alcohol intake, and start incorporating physical activity into your daily routine if you haven’t already. These changes can improve surgery outcomes and your overall health.
-
Medication Review
Your healthcare provider will review your medications. You may need to stop or adjust some medicines before surgery, such as blood thinners or medications for diabetes.
-
Support System
Building a support system with family, friends, or a weight loss group can provide the encouragement and understanding you'll need during this journey.
-
Pre-Surgery Diet
You'll likely be asked to follow a specific diet in the weeks before surgery to reduce surgical risks and prepare your body for the changes it will undergo.
-
Arrangements for Recovery
Plan for time off work, and arrange for help at home if needed. Consider how you'll manage tasks that may be difficult during your recovery.
-
Preoperative Instructions
Follow your surgeon's instructions regarding fasting, medication, and what to bring to the hospital on the day of your surgery. Proper preparation can not only help ensure a smoother surgery and recovery but also help you start on the path to a healthier lifestyle that you'll continue post-surgery.
The Procedure
Bariatric surgery includes a variety of procedures, each with a unique approach to facilitating weight loss. The following are a simplified outline of what the procedures commonly entail:

-
Gastric Bypass (Roux-en-Y)
Surgical Approach: The stomach is divided into a small upper pouch and a larger lower remnant. The small intestine is rearranged to connect to both.
How it Works: It reduces the amount of food that can be consumed and decreases nutrient absorption. -
Sleeve Gastrectomy
Surgical Approach: A large portion of the stomach is removed, leaving a tube-shaped stomach about the size of a banana.
How it Works: It significantly reduces the size of the stomach and decreases the hunger hormone, ghrelin. -
Adjustable Gastric Band
Surgical Approach: A band is placed around the upper part of the stomach to create a small pouch to hold food.
How it Works: The band's tightness can be adjusted for slowing down food consumption and creating an earlier sensation of fullness. -
Biliopancreatic Diversion with Duodenal Switch
Surgical Approach: A more complex procedure that starts with a sleeve gastrectomy and then bypasses a significant portion of the intestine.
How it Works: It significantly reduces the size of the stomach and the amount of nutrients and calories the body absorbs.
What Happens During Surgery?
-
Anesthesia
The patient is put under general anesthesia for the duration of the surgery to ensure they are asleep and pain-free.
-
Incision
Depending on the type of surgery, the surgeon may opt for an open approach, which involves a large incision, or more commonly, laparoscopic surgery, which is minimally invasive and involves small incisions.
-
Modification
The surgical team modifies the stomach and, in some procedures, the small intestine to limit food intake and nutrient absorption.
-
Monitoring
Throughout the procedure, the patient’s vital signs are closely monitored for safety.
-
Closing Incisions
The incisions are stitched or sealed with surgical glue and covered with dressings.
-
Recovery
After the surgery, patients are moved to a recovery area to be closely monitored as they come out of anesthesia.
Benefits of Bariatric Surgery
-
● Significant weight loss
● Improvement or resolution of type 2 diabetes
● Lowered blood pressure and improvement in heart health
● Relief from obstructive sleep apnea
● Reduced joint pain and enhanced mobility
● Improvement in fertility during childbearing years
Recovery and Aftercare
-
● A graduated diet starting with liquids and moving to solid food
● Regular follow-up appointments for monitoring
● Vitamin and mineral supplementation
● Long-term dietary changes and physical activity
Cost and Insurance Information in India
Risks and Considerations
Like all surgeries, bariatric surgery comes with potential risks, such as:
- Nutrient deficiencies due to altered digestion and absorption
- Potential need for a follow-up surgery
- Risk of weight regain if lifestyle changes are not maintained
- Complications such as bleeding, infection, and adverse reactions to anesthesia

