Introduction to Gallbladder Surgery
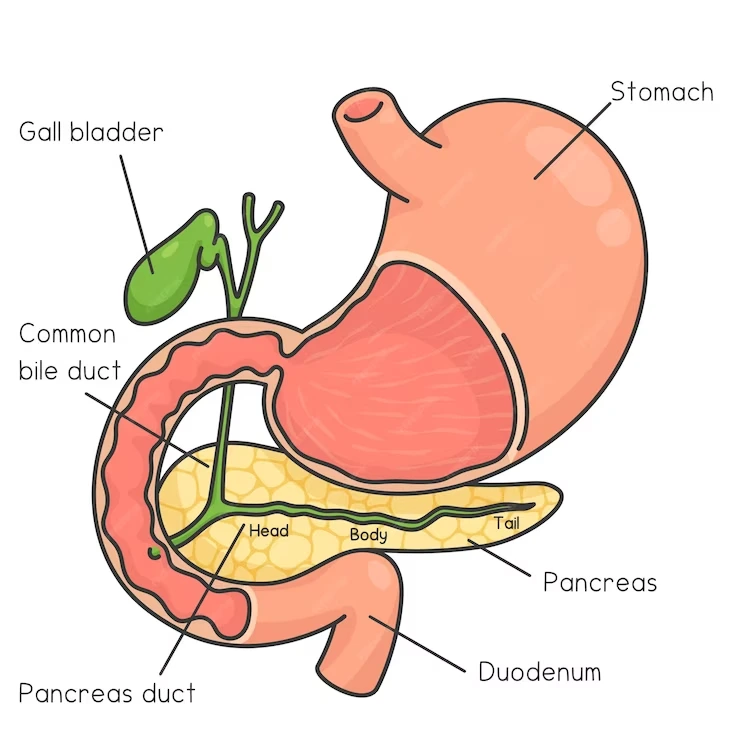
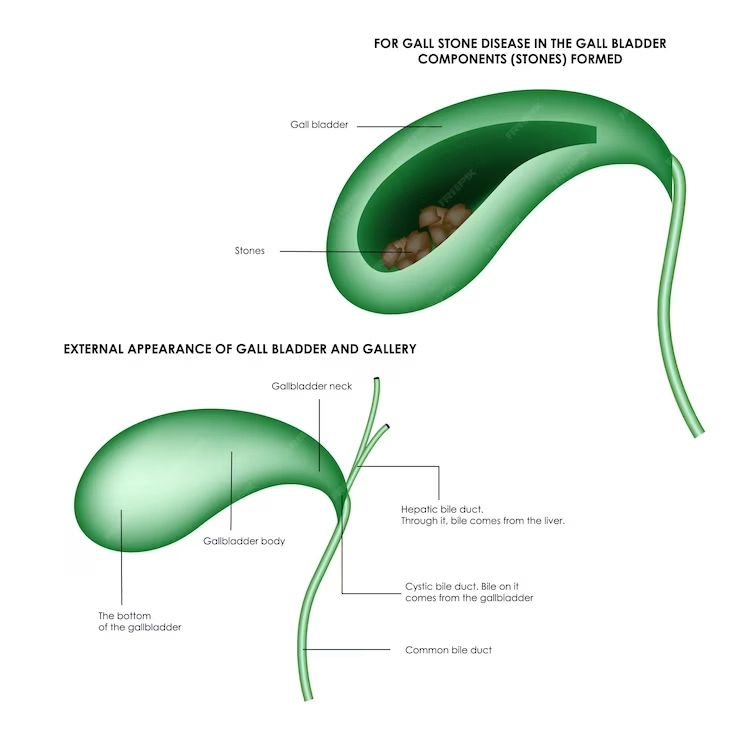
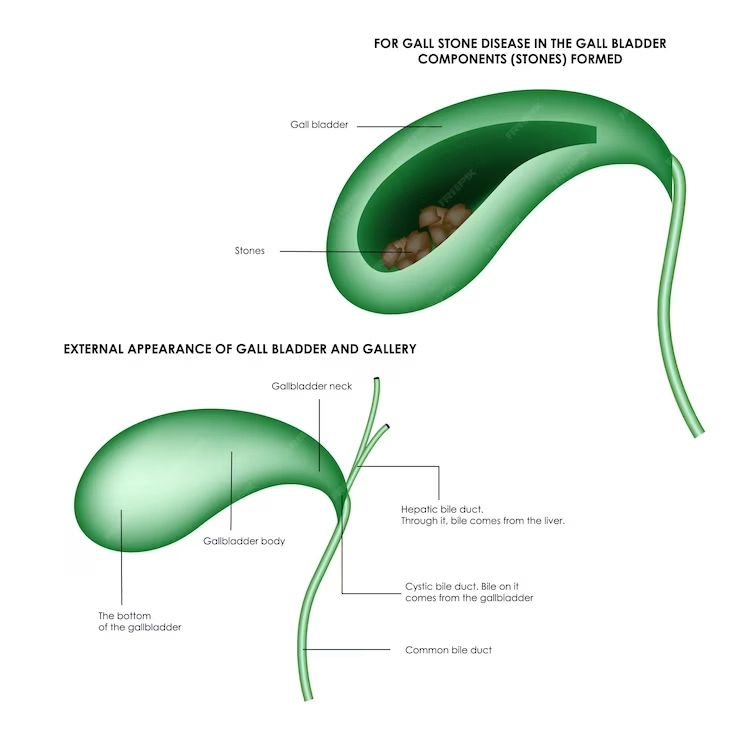
This surgery is typically recommended when a patient suffers from gallstones—hardened deposits of digestive fluid that can cause pain and block the flow of bile—or other gallbladder-related issues, such as inflammation (cholecystitis), pancreatitis, or cholangitis.
Advancements in medical procedures have made gallbladder surgery a routine operation with a high success rate.
The decision to undergo gallbladder surgery is based on several factors, including the severity and frequency of symptoms, the presence of complications from gallstones, and the overall health of the patient. Understanding the function of the gallbladder, the reasons for its removal, and the benefits versus the risks of the procedure can help patients make an informed decision about their treatment.
Understanding Gallbladder Problems
The gallbladder is a crucial component in the digestive system, but it’s prone to a range of issues, most commonly gallstones, which are crystalline formations that develop when bile contains excessive cholesterol or bilirubin.
Gallbladder problems can also stem from inflammation, infection, or biliary dyskinesia, where the gallbladder doesn’t empty bile correctly.
Symptoms of gallbladder issues can include sharp pain in the upper right abdomen, nausea, vomiting, and digestive disturbances, particularly after eating fatty or greasy foods.
These symptoms often lead to a diagnosis via ultrasound or other imaging techniques that confirm the presence of gallstones or other abnormalities.
Understanding the nature of gallbladder problems is vital in determining the appropriate treatment. In many cases, removing the gallbladder is the most effective way to alleviate symptoms and prevent future complications. This understanding helps patients grasp the importance of addressing gallbladder issues promptly and may ease concerns about the necessity of surgery.
Symptoms That Indicate Gallbladder Issues
-
Biliary Colic
This is characterized by a sudden onset of pain in the upper right abdomen or the center of the abdomen below the breastbone. The pain can be severe and may radiate to the right shoulder or back.
-
Jaundice
A yellowing of the skin and whites of the eyes can occur if the flow of bile is blocked, typically by gallstones.
-
Changes in Urine and Stool
Dark urine and light-colored stools may indicate a blockage in the bile ducts.
-
Nausea and Vomiting
These symptoms can accompany a gallbladder attack, especially after eating fatty foods, which can trigger more intense pain and discomfort.
-
Fever and Chills
If there is an infection in the gallbladder, such as cholecystitis, fever and chills may occur.
-
Chronic Digestive Problems
Symptoms like bloating, indigestion, and increased gas can be related to chronic gallbladder disease.
-
Acute Pancreatitis
If a gallstone blocks the bile duct leading to the pancreas, inflammation of the pancreas (pancreatitis) may result, characterized by intense abdominal pain and digestive upset.
Diagnostic Procedures for Gallbladder Dysfunction
-
Medical History and Physical Exam
Initially, doctors will ask about the patient's symptoms, dietary habits, and personal and family medical history. During the physical exam, the doctor may check for pain in the abdomen, particularly in the upper right side, or attempt to detect gallbladder swelling.
-
Blood Tests
Tests can detect signs of infection, inflammation, jaundice, or blockages caused by gallbladder-related problems.
-
Ultrasound
This is the most common imaging test used to look for gallstones or signs of inflammation in the gallbladder.
-
Computed Tomography (CT) Scan
A CT scan provides detailed cross-sectional images of the body and can show gallstones or inflammation.
-
Hepatobiliary Iminodiacetic Acid (HIDA) Scan
This nuclear imaging test tracks the production and flow of bile from the liver to the small intestine and can show obstructions.
-
Medical History and Physical Exam
Initially, doctors will ask about the patient's symptoms, dietary habits, and personal and family medical history. During the physical exam, the doctor may check for pain in the abdomen, particularly in the upper right side, or attempt to detect gallbladder swelling.
-
Blood Tests
Tests can detect signs of infection, inflammation, jaundice, or blockages caused by gallbladder-related problems.
-
Ultrasound
This is the most common imaging test used to look for gallstones or signs of inflammation in the gallbladder.
-
Computed Tomography (CT) Scan
A CT scan provides detailed cross-sectional images of the body and can show gallstones or inflammation.
-
Hepatobiliary Iminodiacetic Acid (HIDA) Scan
This nuclear imaging test tracks the production and flow of bile from the liver to the small intestine and can show obstructions.

-
Magnetic Resonance Imaging (MRI)
MRI scans can visualize the bile ducts and are particularly useful in detecting bile duct blockages.
-
Endoscopic Retrograde Cholangiopancreatography (ERCP)
During this procedure, a flexible tube with a camera (endoscope) is inserted down the throat, through the stomach, and into the small intestine. A dye is injected into the bile ducts, which can then be seen on X-rays.
-
Cholecystokinin (CCK) HIDA Scan
This variation of the HIDA scan checks how well the gallbladder is functioning by measuring the emptying of the gallbladder after administration of a hormone called cholecystokinin.
-
Endoscopic Ultrasound (EUS)
Combining endoscopy and ultrasound, this test can produce detailed images of the gallbladder and surrounding organs.
-
Gallbladder Radionuclide Scan
This test checks for acute cholecystitis or bile duct blockage. A radioactive material is injected into a vein and is tracked as it moves through the liver, gallbladder, and intestine.
What is Cholecystectomy?
Types of Cholecystectomy:
-
1. Laparoscopic Cholecystectomy
This is the most common and minimally invasive method where surgeons make several small incisions to insert a laparoscope (a thin tube with a camera) and specialized instruments to remove the gallbladder.
-
2. Open Cholecystectomy
In cases where laparoscopic surgery is not possible or if complications arise during a laparoscopic procedure, an open cholecystectomy is performed. This involves a larger incision in the abdomen to access and remove the gallbladder.
Procedure Overview
-
Preparation: Patients undergo preoperative tests and are advised to fast before surgery. Anesthesia is administered before the procedure begins.
Incisions:For laparoscopic cholecystectomy, 3-4 small incisions are made. For an open procedure, a single larger incision is made in the abdomen.
Removal of the Gallbladder:The gallbladder is separated from the liver and bile ducts and then removed through one of the incisions.
Closure:Incisions are closed with sutures or surgical staples. In a laparoscopic procedure, a drain may be temporarily placed to remove excess fluids.
Recovery:Laparoscopic surgery typically allows for a quicker recovery with less pain and smaller scars compared to an open procedure.
Postoperative Care
- Patients may return home the same day (laparoscopic) or require a short hospital stay (open surgery).
- Pain management, wound care, and activity restrictions are important aspects of recovery.
- Follow-up appointments are necessary to monitor healing and discuss any dietary modifications.
-
Undergoing a cholecystectomy can significantly alleviate the pain and complications associated with gallbladder stones and other gallbladder diseases.
It's a well-established procedure with a high success rate that has become standard practice for dealing with problematic gallbladder conditions.
Types of Gallbladder Surgery
Types of Cholecystectomy:
-
1. Open Cholecystectomy
Procedure Overview: This traditional method involves a single large incision in the abdomen to access and remove the gallbladder.
When it's Preferred: It's typically reserved for situations where laparoscopic surgery is not advisable, such as when the gallbladder is severely inflamed, infected, or scarred from previous surgeries.
Recovery: Recovery from open cholecystectomy is generally longer, requiring a hospital stay of 2-7 days and several weeks of at-home recovery.
Types of Cholecystectomy:
-
2. Laparoscopic Cholecystectomy
Procedure Overview: This minimally invasive approach uses several small incisions through which a laparoscope (a long, thin tube with a high-resolution camera at the front) and surgical instruments are inserted to perform the surgery.
Advantages:It usually results in less postoperative pain, shorter hospital stays, faster recoveries, and smaller scars.
Recovery: Most patients go home the same day or the following day and can return to normal activities more quickly than with open surgery.
Choice of Procedure
The choice between open and laparoscopic cholecystectomy depends on several factors, including the patient’s medical history, the complexity of the case, and the surgeon’s expertise.
Laparoscopic cholecystectomy is the gold standard and most common method due to its reduced recovery time and less invasive nature.
However, in some complex cases, or if complications arise during a laparoscopic procedure, an open cholecystectomy may be necessary.
Postoperative Considerations
-
Monitoring:Both procedures require careful monitoring for potential complications such as bile leakage or infection.
Lifestyle Changes: After either type of surgery, dietary modifications may be recommended to aid digestion, as the bile will flow directly into the small intestine rather than being stored in the gallbladder.
By understanding the types of gallbladder surgery available, patients can have informed discussions with their healthcare providers about the risks, benefits, and expected outcomes of their surgical options.
Preparing for Gallbladder Surgery
-
Preoperative Evaluation:
Medical Assessment : You will undergo a comprehensive medical evaluation to ensure you're fit for surgery. This may include blood tests, imaging studies, and other diagnostic tests.
Medication Review : Inform your surgeon about all the medications and supplements you're taking, as some may need to be paused or adjusted before the surgery. -
Fasting:
You'll be required to fast, typically for about 12 hours before the surgery, to ensure your stomach and intestiles are empty, which is important for general anesthesia.
-
Bowel Preparation:
Your doctor may prescribe a bowel prep routine to clear your intestines. Follow the instructions carefully.
-
Planning for Recovery:
Support System : Arrange for someone to drive you home after the surgery and help you during the initial recovery phase.
Aftercare Essentials: Prepare your home with items that can assist in recovery, such as ice packs for incisional pain and loose clothing that won’t press on your abdomen. -
Home and Work Arrangements:
Take care of any work obligations or home responsibilities in advance, since you'll need to rest and won't be able to perform strenuous activities for a while.
-
Preoperative Instructions:
Hygiene: You may be asked to shower using an antibacterial soap the night before and the morning of the surgery.
Clothing: Wear comfortable, loose-fitting clothes on the day of your surgery. -
Discussing Anesthesia:
You'll meet with an anesthesiologist to discuss the anesthesia process and any potential risks.
-
Questions and Concerns:
Write down any questions or concerns you may have to discuss with your surgeon before the procedure.
The Gallbladder Surgery Procedure
-
1. Anesthesia
The procedure begins with the administration of general anesthesia, rendering you unconscious and unable to feel pain during the operation.
-
2. Incision and Access
In a laparoscopic cholecystectomy, the surgeon makes several small incisions in the abdomen to insert a laparoscope (a thin tube with a camera) and specialized surgical tools.
For an open cholecystectomy, a single, larger incision is made in the abdomen to access the gallbladder directly. -
3. Gallbladder Removal
The surgeon carefully separates the gallbladder from the liver and other structures. Key steps include clipping the cystic duct and artery, and then removing the gallbladder.
In laparoscopic surgery, the gallbladder is removed through one of the small incisions.
-
4. Examination and Cleaning
The surgeon examines the area for any potential bile leakage and ensures that the remaining ducts are intact and secure.
The area is cleaned and any excess bile is removed. -
5. Incision Closure
For laparoscopic surgery, the incisions are closed with sutures or staples and covered with dressings.
In an open procedure, the larger incision is closed with sutures or staples, and a drain may be placed to prevent fluid accumulation. -
6. Recovery
After the surgery, you will be taken to a recovery area to be closely monitored as you wake from anesthesia.
Most laparoscopic cholecystectomy patients can go home the same day, while open surgery may require a hospital stay. -
7. Postoperative Instructions
You will receive instructions on how to care for your incisions, signs of complications to watch for, and guidelines on diet and activity restrictions.
Recovery and Postoperative Care
-
1. Immediate Postoperative Period
In the case of laparoscopic surgery, patients often go home on the same day. With an open cholecystectomy, a hospital stay of 2 to 4 days is typical.
You'll receive pain management assistance and may have a catheter placed to drain urine. -
2. Pain Management
You will experience some pain and discomfort, which can be managed with medications prescribed by your doctor.
For laparoscopic surgery, shoulder pain can occur due to the CO2 gas used; it usually dissipates within a couple of days.
-
3. Incision Care
Keep the surgical site clean and dry. Instructions on how to bathe will be provided.
If sutures or clips are used, they may need to be removed during a follow-up visit. -
4. Activity and Rest
Rest is crucial; however, short, gentle walks are encouraged to aid circulation and prevent blood clots.
Avoid heavy lifting or strenuous activity for a period as advised by your surgeon, usually about four to six weeks for open surgery and one to two weeks for laparoscopic surgery. -
5. Diet
You may start with liquids and soft foods as tolerated before progressing to your regular diet.
Some may experience changes in bowel habits or digestion. A low-fat diet is often recommended initially. -
6. Monitoring for Complications
Watch for signs of infection, such as increased redness, swelling at the incision site, fever, or drainage.
Report any severe abdominal pain, jaundice, or persistent vomiting to your doctor. -
7. Follow-Up Appointments
Attend all scheduled appointments so your doctor can monitor your recovery and address any concerns.
-
8. Long-Term Care
Most people return to normal activities within a week after laparoscopic surgery and within 4-6 weeks after open surgery.
Discuss with your doctor when it's safe to resume driving, working, and exercising. -
9. Lifestyle Adjustments
While the gallbladder is not essential for living, some dietary adjustments can help maintain digestive comfort.
Staying active, maintaining a healthy weight, and eating a balanced diet high in fiber and low in saturated fats can be beneficial. -
10. Support and Resources
Seek support from family and friends during recovery, as emotional well-being is an important part of healing.
If needed, your healthcare provider can also connect you with postoperative support groups or counseling services.
Risks and Potential Complications
-
1. General Surgical Risks
Infection: Surgical site infections can occur, signaled by redness, swelling, or discharge.
Bleeding: While uncommon, excessive bleeding may happen during or after surgery.
Adverse reactions to anesthesia: Some individuals may have an unexpected response to anesthesia, though serious reactions are rare. -
2. Specific Risks Associated with Gallbladder Surgery
Bile leak : Bile may leak into the abdominal cavity, potentially requiring additional procedures.
Bile duct injury: There's a small risk that the bile ducts could be damaged, which might need corrective surgery.
Intestinal injury: During the surgery, other organs or the intestines may be inadvertently injured.
-
3. Postoperative Complications
Blood clots: Immobility after surgery can increase the risk of developing blood clots, particularly in the legs (deep vein thrombosis).
Pneumonia: Breathing exercises and mobility are encouraged to prevent respiratory complications like pneumonia. -
4. Long-Term Complications
Changes in digestion: Some patients might experience changes in their digestion or bowel habits.
Postcholecystectomy syndrome: Symptoms similar to gallbladder attacks may continue in some individuals after surgery.
Incisional hernia: There's a possibility of a hernia at the incision site, particularly after open surgery. -
5. Psychological Impact
Adjustment issues: Some patients may need time to adjust to lifestyle and dietary changes post-surgery.
-
6. Risks for Specific Populations
Elderly patients or those with comorbidities: There may be an increased risk of complications for these individuals.
● Using prophylactic antibiotics to prevent infection.
● Encouraging movement to reduce the risk of blood clots.
● Monitoring during surgery to minimize the risk of bile duct and other organ injuries.
If you experience any signs of complications, such as severe pain, fever, jaundice, persistent nausea, or vomiting after the surgery, it is crucial to contact your healthcare provider immediately. Early intervention can prevent more serious complications and promote better outcomes.
Life After Gallbladder Removal
-
1. Dietary Adjustments
Initially, you may need to eat a low-fat diet to allow your body to adapt to digesting fat without the gallbladder's bile reserve.
Gradually, you can reintroduce more foods and observe how your body responds to them. -
2. Digestive Changes
some people experience changes in bowel habits, such as diarrhea or more frequent bowel movements, particularly after eating fatty foods.
These symptoms are usually temporary and often settle down over time as the body adjusts. -
3.Bile Flow Changes
Without a gallbladder, bile flows directly from the liver into the small intestine. This can lead to a more continuous, rather than concentrated, release of bile.
-
4. Nutritional Considerations
You may need to be more mindful of getting enough fat-soluble vitamins (A, D, E, K) and essential fatty acids, as bile is essential for their absorption.
-
5. Physical Activity
Most patients can return to their normal activities within a week or two after laparoscopic surgery, while open surgery may require a longer recovery time.
Regular exercise can help improve overall digestion and health.
-
6. No Need for Routine Check-Ups
Generally, unless you have complications, there is no need for regular medical follow-ups just for the absence of the gallbladder.
-
7. Monitoring for Postcholecystectomy Syndrome
A small percentage of patients may experience postcholecystectomy syndrome, which includes symptoms similar to those that occur with gallstones. If this happens, consult your doctor for management strategies.
-
8. Long-term Health
Removing the gallbladder doesn't shorten your life expectancy. In fact, it can significantly improve quality of life if you were experiencing painful symptoms before.
-
9. Emotional Health
As with any surgery, feelings of anxiety or depression post-surgery are possible. Support from healthcare professionals, friends, and family can be beneficial.
-
10. Adjusting Expectations
While most patients won't notice significant changes in their lifestyle, it's important to have realistic expectations and give the body time to adapt.
Diet and Lifestyle Changes Post-Gallbladder Surgery
-
1. Gradual Dietary Shifts
Start with a clear liquid diet immediately after surgery to allow your digestive system to rest.
Slowly progress to a bland diet with items like toast, rice, and bananas before introducing regular foods. -
2. Low-Fat Diet
Initially, focus on low-fat foods to reduce the workload on your liver and intestines.
Gradually reintroduce healthy fats like avocados, nuts, and olive oil over several weeks, monitoring your body's response. -
3. Smaller, Frequent Meals
Eating smaller, more frequent meals can help manage the continuous flow of bile into your intestines and prevent discomfort.
-
4. Hydration
Drink plenty of water throughout the day to help digestion and maintain hydration.
-
5. Fiber Intake
A fiber-rich diet helps regulate bowel movements and prevents diarrhea, which can sometimes occur after surgery.
Increase fiber gradually to avoid gas and bloating. -
6. Avoiding Certain Foods
Spicy and highly processed foods may cause discomfort for some individuals after gallbladder removal.
Foods and beverages that can cause gas, such as beans, cabbage, and carbonated drinks, may also need to be minimized. -
7. Physical Activity
Incorporate regular physical activity to maintain a healthy weight and improve digestion.
Start with light walking and gradually increase the intensity as your recovery progresses. -
8. Alcohol and Caffeine
Limit or avoid alcohol and caffeine during the recovery period, as they can strain the digestive system.
-
9. Vitamin Supplementation
Discuss with your doctor if you need supplements, especially for fat-soluble vitamins that may not be absorbed as effectively without concentrated bile.
-
10. Long-term Lifestyle Considerations
A balanced diet rich in fruits, vegetables, lean proteins, and whole grains supports long-term health.
Regular check-ups with your doctor can help monitor your health and address any dietary concerns. -
11. Emotional Well-being
Recovery can also be an emotional process. Seek support from friends, family, or professional counselors if needed.
-
12. Listen to Your Body
Each person’s reaction to surgery is different. Pay attention to how your body responds to dietary and lifestyle changes, and adjust accordingly.
Cost and Insurance Coverage for Gallbladder Surgery in India
-
1. Type of Surgery: The choice between laparoscopic and open cholecystectomy impacts cost. Laparoscopic surgery, though less invasive, might be more expensive due to the technology used.
2. Hospital Selection:
Private hospitals, especially those catering to medical tourism, might charge more compared to government hospitals.
Facilities accredited by organizations like JCI (Joint Commission International) or NABH (National Accreditation Board for Hospitals & Healthcare Providers) might have different pricing structures.
3. Surgeon’s Expertise: - The cost can be influenced by the surgeon's experience and reputation. Renowned surgeons or specialists in the field may charge higher fees.
4. Location: - Metropolitan cities like Mumbai, Delhi, Bangalore, and Chennai may have higher medical costs compared to smaller cities or towns.
5. Pre- and Post-Operative Care: - Pre-operative consultations, diagnostic tests, and post-operative care including medications and follow-up visits add to the overall cost.
6. Insurance Coverage:
Many health insurance policies in India cover gallbladder surgery, but it is essential to check the terms and conditions, as coverage may vary.
There may be limitations on room rent, surgery costs, and types of procedures covered.
Some policies might have waiting periods before you can claim benefits for surgical procedures.
-
7. Additional Costs:
Consider potential unforeseen expenses such as extended hospital stays, complications, or additional treatments.
Some insurances may not cover ancillary charges such as a private recovery room or special nursing care.
8. Cashless Facility: - Some hospitals offer a cashless facility for patients with health insurance, meaning the hospital will directly settle the bill with the insurance provider, subject to policy terms.
9. Government Schemes: - Government health schemes may cover gallbladder surgery for eligible individuals, significantly reducing out-of-pocket expenses.
10. Price Transparency: - It’s advisable to seek detailed billing estimates from hospitals beforehand to avoid hidden charges.
11. Negotiating Medical Bills: - In some cases, there is room to negotiate medical bills, especially in private hospitals where package deals for surgery might be available.
12. EMI Options: - Many hospitals have started offering EMI (Equated Monthly Installment) options for patients who cannot afford to pay the entire fee upfront.
-
It's crucial for patients to have a clear understanding of their financial responsibilities before proceeding with gallbladder surgery. Consulting with the hospital's billing department and insurance provider can offer clarity on coverage limits and out-of-pocket expenses. Patients should also explore all options, such as government aid if they meet eligibility criteria, to reduce the financial burden of the surgery.
Choosing the Right Surgeon for Gallbladder Surgery
-
Credentials and Experience
Verify the surgeon's qualifications, ensuring they are board-certified and trained specifically in gastrointestinal and gallbladder surgeries. Look for a surgeon with extensive experience in performing the specific type of gallbladder surgery you require, whether it's laparoscopic or open cholecystectomy.
-
Hospital Affiliations
Consider surgeons who are affiliated with hospitals that have a good reputation for care quality and have the necessary infrastructure for handling complications should they arise.
-
Surgical Success Rate
Inquire about the surgeon's success rate with gallbladder surgeries. High success rates can be indicative of the surgeon's proficiency and reliability.
-
Patient Reviews and Testimonials
Reading through patient reviews and testimonials can provide insights into the surgeon's approach and patient satisfaction.
-
Consultation
Schedule a consultation with the surgeon to discuss your condition and the procedure. This meeting can give you a sense of their communication style and willingness to address your concerns.
-
Second Opinion
Don’t hesitate to seek a second opinion. It can provide you with additional perspectives on the best surgical options and the necessity of the procedure.
-
Insurance Network
Check if the surgeon is within your insurance network, which can affect your out-of-pocket costs.
-
Technology and Technique
Choose a surgeon who is adept at using the latest technology and surgical techniques, which can lead to better outcomes and shorter recovery times.
-
Post-Operative Care
Find out about the follow-up care protocol the surgeon provides. Good post-operative care is crucial for a speedy recovery.
-
Team and Support Staff
Consider the quality and responsiveness of the surgeon's team, including nurses and administrative staff, as they will be part of your care.
-
Hospital's Surgical Volume
Research shows that hospitals and surgeons who perform a higher volume of certain procedures often have better outcomes.
-
Communication
The ability of the surgeon to communicate complex information in an understandable way is essential. You should feel comfortable asking questions and confident in the responses you receive.
-
Accessibility
The surgeon should be accessible for any pre-surgery consultations and for follow-up after the procedure.

